Increase Primary Medication Adherence
And Improve Outcomes for More Patients
The Stubborn Primary Adherence Challenge
The main goal of healthcare professionals is helping patients back to wellness. And when it comes to outpatients with acute illnesses the path to wellness should be as short as possible. In the US this usually means prescribing medications: 74-80% of ER and outpatient visits result in drug therapy.1
So once a patient gets a prescription, all that he or she has to do is just fill it to start feeling better. Pretty simple, right? The reality is more complicated.
Research shows that 20-30% of all new prescriptions written NEVER get filled by patients.2,3
Despite the explosion of new retail pharmacy stores, mail order drugs and addition of onsite walk-in clinics at chain pharmacies, primary non-adherence hasn’t budged.4
The High Costs of Non-Adherence
This failure to fill new prescriptions – called primary non-adherence to medications – is a significant driver in the national non-adherence epidemic of staggering proportions. In its broadest terms medication adherence is defined as a process that begins with the receipt of the medication, continues with correct usage and repeats with refills, if necessary.5
Some estimates put the number of patients not taking chronic medications as high as 50% while others state that as much as half of all prescriptions may not be taken.6
While the effects of primary non-adherence have not been studied exclusively, the fact that up to 30% of all prescriptions are not picked up makes primary non-adherence a large group in the overall non-adhering population.
Non-adherence in all its forms imposes high costs on healthcare providers, payers and the society at large.
- The IMS Institute of Healthcare Informatics estimates that improving medication adherence would eliminate at least $105 billion in avoidable healthcare costs in the US.7
- Poor outcomes resulting from non-adherence can impact other economic factors such as employee productivity. In a study of 10 employers with a total of 51,648 employee respondents, researchers found that health-related productivity losses were estimated to be 2.3 times higher than direct healthcare costs.8
- And while recently a great deal of public attention has focused on the rising prices of medications in the US, one study estimated the annual cost of prescription drug-related morbidity and mortality resulting from non-optimized medication therapy, including medication non-adherence, to be $528.4 billion in 2016 US dollars, with a plausible range of $495.3 billion to $672.7 billion.9
“Drugs don’t work in patients who don’t take them”, said C. Everett Koop, MD, who was widely regarded as the most influential Surgeon General in American history for his role in changing public attitudes about smoking.
Patients who fail to pick up prescriptions are much more likely to end up sicker and need additional care. Given the magnitude of primary non-adherence, drugs certainly don’t work in people who never fill their prescriptions.
Patient Jobs: Healthcare's Best-Known Secret
So why do so many outpatients fail to pick up prescriptions and undermine their own recoveries? Researchers studying the topic have acknowledged challenges with identifying and measuring the patient behaviors that drive primary non-adherence.5
Dr. Ken Rosenblum, who founded InstyMeds, approached non-adherence from the patient’s perspective.
As an Emergency Room physician he had an insider’s understanding of some obvious but overlooked causes of non-adherence. He saw that sending patients on a quest for medications, regardless of their physical or mental state and mobility challenges, resulted in suboptimal filling of prescriptions.
Dr. Rosenblum realized that in our healthcare system prescribing medications to patients also meant giving them a job to do.
Their job – never mentioned because it’s universally implied – is to get to a pharmacy and wait for their prescriptions to be filled before they can start their medications. It’s a job whose critical importance in the recovery process is taken for granted due to its seemingly trivial nature. Yet, for patients who are sick, tired, in pain or those caring for sick children and dependents, it’s the last thing they want to be doing.
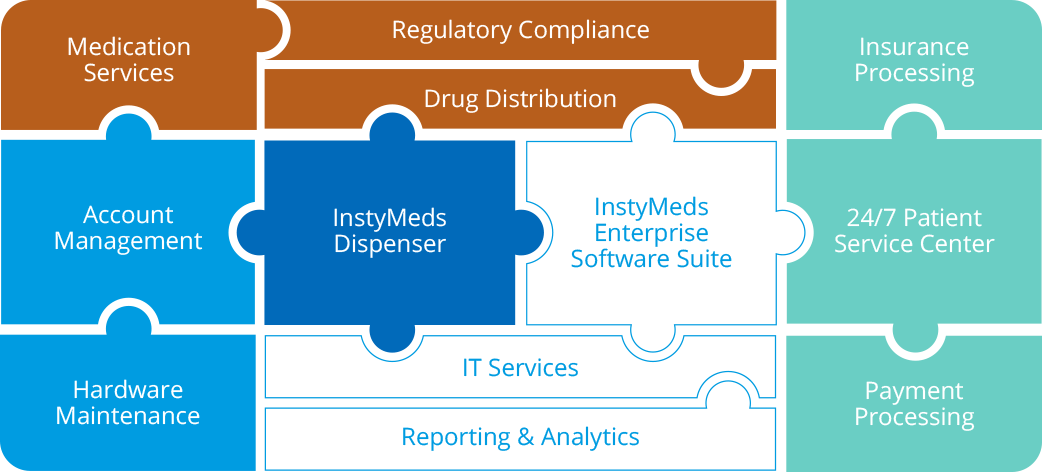
InstyMeds: Eliminate Patient Jobs to Improve Adherence and Outcomes
InstyMeds eliminates patient jobs by allowing patients to pick up prescriptions at the point of care. A patient can get all her medications quickly from an InstyMeds dispenser right after leaving her provider’s office and start feeling better faster!
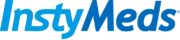
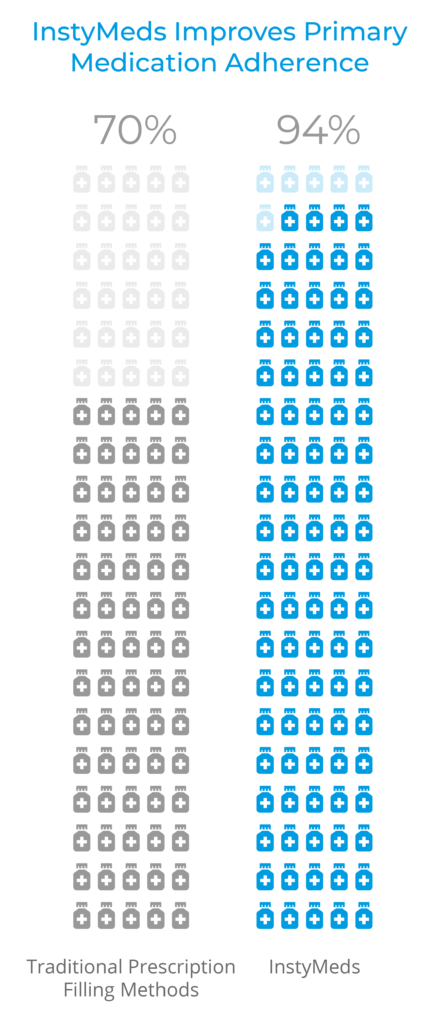
And when providers make picking up prescriptions so easy, patients almost always do:
94% of aggregate InstyMeds prescriptions are filled, significantly exceeding the industry average of 70%.
Practice shows that when more patients fill their medications, outcomes improve. This was demonstrated by a study at the University of Maryland Medical Center10 as well as by our own 2019 InstyMeds Outcomes Study:
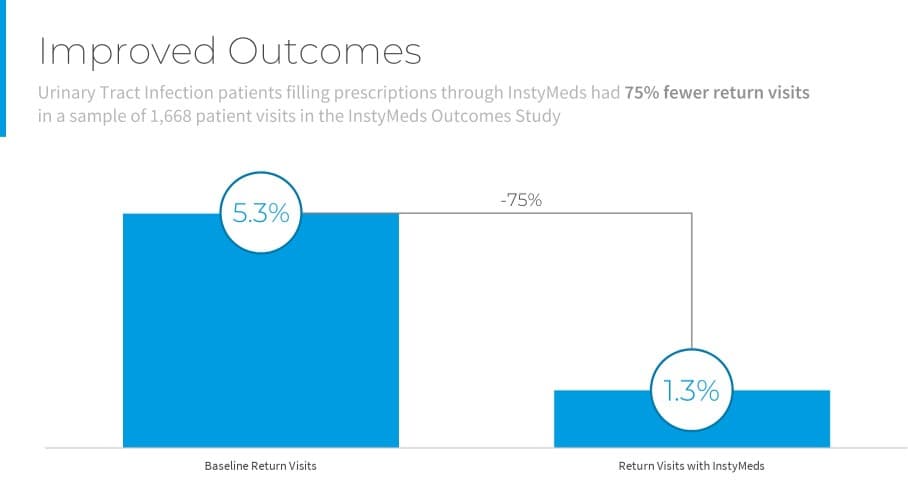
- The InstyMeds Outcomes Study analyzed return visit rates (within 2 weeks) for a sample of 1,668 patients with urinary tract infections (UTI).
- Patients who received antibiotic prescriptions to InstyMeds returned to the ED at a rate of 1.3%, compared to that of 5.3% for the control population.
InstyMeds demonstrated a 75% reduction in return visits for patients with UTI diagnosis. In other words, improving primary adherence led to improved outcomes.
Learn More About Direct-to-Patient Dispensing
Interested in learning more?
1 U.S. Centers for Disease Control and Prevention.
2 Fischer, M. A., et al. (2011). “Trouble getting started: predictors of primary medication nonadherence.”
3 Tamblyn, R., et al. (2014). “The Incidence and Determinants of Primary Nonadherence With Prescribed Medication in Primary Care A Cohort Study Primary Nonadherence With Prescribed Medication in Primary Care.”
4 DiMatteo, M. R. (2004). “Variations in Patients’ Adherence to Medical Recommendations: A Quantitative Review of 50 Years of Research.”
5 Solomon, M. D. and S. R. Majumdar (2010). “Primary non-adherence of medications: lifting the veil on prescription-filling behaviors.”
6 “The Cost of Not Taking Your Medicine” by Jane E. Brody; The New York Times, April 17, 2017.
7 IMS Institute for Healthcare Informatics (2013). “Avoidable Costs in U.S. Health Care.”
8 Loeppke, R., et al. (2009). “Health and productivity as a business strategy: a multiemployer study.”
9 Watanabe, J. H., et al. (2018). “Cost of Prescription Drug-Related Morbidity and Mortality.”
10 Hayes, B. D., et al. (2012). “To-Go medications for decreasing ED return visits.” The American Journal of Emergency Medicine 30(9): 2011-2014.